Dental Education
Fluoride SupplementsThe most effective way for your child to get fluoride’s protection is by drinking water containing the right amount of the mineral… about one part fluoride per million parts water. This is of special benefit to children, because fluoride is incorporated into enamel as teeth form. Children who, from birth, drink water containing fluoride have up to 40% fewer cavities. Many of them remain cavity-free through their teens. |
 |
| Fluoride is one of the most effective elements for preventing tooth decay. This mineral combines with tooth enamel to strengthen it against decay. Fluoride may also actually reverse microscopic cavities by enhancing the process by which minerals, including calcium, are incorporated into the teeth. Even though your regular water supply may be fluoridated, it is still important to discuss with your dentist any additional fluoride needs your child may have. Look for fluoride toothpastes and over-the-counter fluoride mouth rinses that carry the ADA seal. They have been proven safe and effective for their intended use. The advertising claims for these products have been reviewed by the ADA so the claims are accurate and not misleading.Your dentist may recommend various ways to get fluoride protection, including: – Drinking fluoridated water at school. – Taking prescribed fluoride tablets or drops. – Brushing with a pea-sized amount of fluoride toothpaste after age two. – Using a fluoride mouth rinse for children over age six. |
|
Types of Mouth GuardsYou don’t have to be a football player to benefit from wearing a mouth protector. Any adult or child involved in a recreational activity that poses a risk of injury to the mouth can obtain smile protection with this important safety device.
Pre-fabricated: A pre-fabricated mouth guard can be purchased at stores, these mouth guards are often only offered in a general size offerings. Custom: Mouth guards can also be fabricated by your dentist using an exact model (impression) of your mouth. This type of mouth guard provides superior fit and protection. |
| Custom-made mouthguardsYour dentist can create a special mouth protector just for you – one that will provide comfort and proper fit. A custom-made mouth protector is individually designed and constructed in the dental office or according to your dentist’s specifications in a professional dental laboratory.
First, the dentist makes an impression of the patient’s teeth. Using a special material, the dentist constructs the mouth protectors over a model of the teeth. Although custom-made mouth protectors are somewhat more expensive than stock mouth protectors purchased in stores, their exceptionally good fit, comfort, and overall quality make them worth it. A custom-made mouth protector is easily retained in the mouth and does not interfere with speech or breathing. For these reason, custom-made devices are often preferred by sports enthusiasts and recommended by dentists. So give your smile a sporting chance – ask you dentist about mouth protectors. |
What Sealants Do for YouA sealant is a clear shaded plastic material that is applied to the chewing surfaces of the back teeth (premolars |
Who Should Have SealantsAlthough children receive significant benefits from sealants, adults can also be at risk for pit and fissure decay and thus be candidates for sealants. Your dentist can advise you about the need for sealants. Sealants are also recommended even for those who receive topical applications of fluoride and who live in communities with |
How Long Do Sealants LastWhen the sealant is applied, finger-like strands penetrate the pits and fissures of the tooth enamel. Although the sealant cannot be seen with the naked eye, the protective effect of these strands continues. As a result, it may be several years before another application of sealant is needed. Reapplication of the sealants will continue the protection against decay and may save the time and expense of having a tooth restored. Sealants will be checked during regular dental visits to determine if reapplication is necessary. |
How Sealants Save MoneyThe American Dental Association recognizes that sealants can play a major role in the prevention of tooth decay. When properly applied and maintained they can successfully protect the chewing surfaces of the tooth from decay. A total prevention program includes brushing twice a day, cleaning between teeth daily with floss or interdental cleaner, regular dental visits, and limiting the number of between-meal snacks. Ask your dentist how to obtain the right level of fluoride. If these measures are followed and sealants are used well, the risk of decay can be reduced or may even be eliminated. |
Aftercare
Twice a day brushing is very important to maximize the benefits of the sealants. Of course, sealants should be |
X-rays
Is it safe to have dental X-rays? How often are they necessary? This depends upon the patients individual health needs. If you are a new patient, the dentist may recommend X-rays to determine the current status of your mouth and to check for hidden problems. The need for radiographs varies according to your age, risk for disease, and your past dental history. Children may need X-rays more often than adults because their teeth and jaws are still developing and they are more prone to tooth decay. X-rays help the dentist discover developmental problems as early as possible so preventative or treatment measures can be started. |
FluorideFluoride is one of the most effective elements for preventing tooth decay. This mineral combines with tooth enamel to strengthen it against decay. Fluoride may also actually reverse microscopic cavities by enhancing the process by which minerals, including calcium, are incorporated into the teeth. The most effective way for your child to get fluorides protection is by drinking water containing the right amount of the mineral… about one part fluoride per million parts water. This is of special benefit to children, because fluoride is incorporated into enamel as teeth form. Children who, from birth, drink water-containing fluoride have up to 40% fewer cavities. Many of them remain cavity-free through their teens. Even though your regular water supply may be fluoride products such as toothpaste, and in some cases, mouthrinses. You may want to discuss with your dentist any special fluoride needs your child may have. Fluoride toothpastes and over-the-counter fluoride mouth rinses that carry the ADA seal have proven safe and effective. Your dentist may recommend various ways to get fluoride protection including: – Drinking fluoridated water at school. – Taking prescribed fluoride tablets or drops – Brushing with a pea-sized amount of fluoride toothpaste. – Using a fluoride mouth rinse for children over age six. |
Parental ResponsibilityWith your help, in combination with their own efforts and regular professional care, your daughters and sons can grow up cavity-free and keep their teeth all their lives. It’s not difficult to help your child maintain a healthy smile. Here are a few tips for good oral health: – Make sure your child gets the fluoride needed for decay-resistant teeth. Ask your dentist how this should be done. – Brush and floss your child’s teeth daily until the child can be taught to do this alone. Then encourage him or her to brush and floss. – Take your child to see the dentist regularly, beginning at six months of age. – Put only water in your child’s nap time or bedtime bottle. – Start cleaning your child’s mouth daily. – Start brushing as soon as the first tooth erupts. |
 |
What is Bonding?Bonding is a term used to describe a number of procedures that involve applying composite resins to the tooth. Regardless of its use, bonding can provide an attractive result. |
How Bonding is PerformedBonding is often completed in one visit and often does not require the use of anesthesia or drilling. The process involves preparing the tooth surface with an etching solution that allow the composite resin to adhere. To match the color of your teeth, various colors of resins are carefully blended so the bonded tooth will look natural. The resin is applied, contoured into the proper shape and hardened using a special light or chemical process. It is smoothed and polished to appear natural. Sometimes a follow-up appointment will be required for final polishing and finishing. |
Aftercare
– Avoid acids (such as vinegar, tomatoes, or pineapples) and alcohol which can damage the resins. – Avoid items that can stain bonding material such as cigarettes, coffee, tea, and berries. – Do not put excess pressure on resins. Chewing ice, popcorn kernels and hard candy can cause damage.
|
What Causes Discoloration?While people have different colors of skin and hair, they also have genetic differences in tooth color. Some teeth are more yellow, while others yellow with aging. Natural tooth color can be discolored by a number of causes. The surface of the teeth can be stained by tobacco, coffee, tea, berries and other foods as well as by deposits of calculus (which is better known as tartar). Discoloration of the tooth internally can also result from aging, injuries, excessive fluoride, certain illnesses and taking antibiotic tetracycline during early childhood. Although bleaching successfully lightens most discolorations, certain types (like those caused by tetracycline) are more difficult to remove. |
 |
Chairside Bleaching
|
|
| Chairside bleaching takes from 30 minutes to one hour per visit. It is not uncommon for the teeth to become slightly sensitive following bleaching treatments. To protect the mouth, a gel-like substance is applied to the gums and a rubber “shield” is placed around the necks of the teeth. A chemical solution, the oxidizing agent, is painted onto the teeth. A special light may be used to activate the agent. | |
 Before |
 After |
| To achieve the best results, teeth may be bleached a shade lighter than the desired since they will tend to darken slightly with time. Generally two to ten visits may be necessary to complete the process of chairside bleaching.(Back to top) | |
In-home BleachingWith in-home bleaching, the dentist makes an impression for a model of the teeth, fabricates a custom-fitted tray and prescribes a bleaching agent that comes in the form of a bleaching gel. The gel is placed in the custom-fitted tray and worn up to two hours daily or at night for about two weeks. The amount of time the custom-fitted tray is worn and the duration may vary according to a person’s individual need and the recommendations of the dentist. The dentist will monitor the entire process of in-home bleaching to assure its effectiveness and safety. Over the counter products that are self-administered are not recommended, although they may appear to cost less. Bleaching treatment should be done under the supervision of a dentist following a proper exam and diagnosis. Whiteners with the ADA Seal of Acceptance have proven to be safe and effective. |

|
Who Can Benefit?Most bleaching procedures last one to three years, although in some situations it may last longer. Some people, with certain dental conditions, may not be good candidates for this type of bleaching. People with gum recession, for example, may have exposed root surfaces that are highly sensitive and could be further irritated by the ingredients in the whiteners or bleaching components. In addition, these products are not recommended for habitual tobacco and alcohol users. Brushing and flossing, twice a day, as well as regular professional cleanings, along with occasional touch-up treatments will help keep teeth white. An attractive smile increases self-confidence. |
How Long Whitening Lasts?Whitening usually lasts between one and three years. However, it is important to: – Brush twice a day – Floss once a day – Have regular cleanings at your dentist’s office – Ask your dentist about any concerns you may have |
Types of Orthodontic CareBefore orthodontic treatment can begin, pre-treatment records are gathered (this is the key to successful diagnosis of orthodontic problems). Those records include medical/dental history, clinical examination, plaster study models of your teeth, photos of your face and teeth and x-rays of your head. This information will be used to decide on the best treatment for you.
|
Removable Dental AppliancesAt the other end of orthodontic treatment, a special appliance is fabricated to hold the teeth in their new positions. This is called a “retainer”. Some retainers are cemented over teeth to hold the position and others that are removable. Other removable appliances are very similar to the removable “retainer” in looks but provide a very different function. These can, in fact, create pressures on teeth in a specific way so as to cause the appropriate teeth to come into the correct position. This appliance can be used for active treatment as well as for post treatment retention. |
Types of BracesBraces come in a variety of shapes, sizes, and colors. Some are the more traditional looking metal brackets that have been greatly reduced in size. Other brackets are clear plastic types and still other are made of ceramic materials. These last two types have been developed to aid in creating a greater cosmetic acceptance by patients in treatment.
Sometimes these brackets can be placed on the inside of the teeth. Brackets positioned in this way cannot be detected by others. |
MalocclusionsClass 1 – Unilateral posterior cross bit, on the right side, slight anterior open bite.
Class 1 – crowding, deep bite
Class 2 division 1 – Crowding, deep bite, adult surgical case
Class 2 division 2 – Deep bite, severe crowding
Class 2 division 2 – Mandibular asymmetry, lateral open bite, posterior cross bite, crowding
|
CleansingYou would probably never dream of not bathing your body but give less thought to not brushing or flossing your teeth. When you have braces, it is incredibly important that you give as much attention to cleaning the braces as you do to cleaning the rest of your body. The bands or bonded brackets on braces create small nooks and crannies where food and plaque (an invisible file of bacteria) can hide. If plaque is allowed to remain on the teeth for a long time, it can increase the likelihood of tooth decay. This same process can also cause permanent white lines and spots as enamel is dissolved by the acids. Because of these problems, it is essential to brush after every meal and snack. You should also clean between your teeth and around each bracket daily. Brushing removes the food and plaque that forms on your teeth. When you brush, use a brush with soft and rounded bristles or a special orthodontic brush and also, use fluoride toothpaste. Look for the American Dental Association’s Seal of Acceptance. The Seal is awarded to products that have proven to be effective. How should I brush? A number of different tooth brushing methods are acceptable. Whichever method you use, take the time to brush thoroughly. Here’s an example of a method: – Place a soft-bristled brush at a 45-degree angle against the gums. – Move the brush back and forth in short strokes with a gentle scrubbing motion. – Brush the inner, then outer, and finally the chewing surfaces of the teeth. – Use the “toe” of the brush to reach the inner front tooth surfaces. – Brush your tongue to help freshen your breath. After brushing, rinse well. Then closely inspect your teeth and braces in a well-lighted mirror. You may have to brush and rinse several times before your teeth are clean. Is flossing possible with braces? Yes! But it can be a little tricky while wearing braces. A floss threader can help you slip the flow between the braces or under the arch-wire. – Once the floss is in place, hold it between your forefingers, about an inch apart. – Using a gentle sawing motion, guide the floss between your teeth. Do not snap it in place. – When the floss reaches the gum-line, cure it against the tooth and gently slide it into the space between the gum and tooth. – When you feel resistance, gently rub the side of the tooth moving the floss away from the gum. – Rinse your teeth to wash away food or other particles that you removed with the floss. Are there other products that can help me clean my mouth? There are several dental aids that can be helpful. Specially shaped brushes, the other interdental cleaners and oral irrigating devices can often help clean some of those hard-to-reach areas. After brushing prior to bedtime, an ADA accepted fluoride mouth-rinse should be used for added protection of the enamel surfaces of the teeth. Interdental Cleaners Interdental cleaning devices with the ADA Seal of Acceptance are specially shaped brushes or other implements that help remove plaque. They are usually made of wood, plastic or rubber and shaped to help clean between the teeth. They can be particularly useful for people who wear braces or who have trouble handling floss. Discuss the proper use of these devices with your dentist to avoid injuring your gums. Oral Irrigators These devices create a focused stream of water to remove particles of food from the surfaces around and between the teeth. They are useful for cleaning hard-to-reach areas and may reduce gingivitis. They are especially helpful for people who have braces. Your dentist will tell you if you can benefit from using this device and provide instruction on proper use. Look for devices bearing the ADA Seal of Acceptance. Fluoride Mouth Rinse Fluoride with the ADA Seal of Acceptance provides extra protection for your teeth. Is an element that combines with tooth enamel, strengthening it against decay. Fluoride can even repair microscopic cavities by helping mineral incorporate into the teeth. You may want to discuss with your dentist the need for additional fluoride products such as non-prescription mouth rinses for children in your family over the age of 6. Dental aids can play an important role in cleaning those hard-to-reach areas, but your diligence in daily cleaning is really the key to good oral health. By watching your diet, practicing good oral hygiene and following your dentist instructions, you can be assured that your orthodontic treatment will be a success. Remember, it is even more important that you visit your general dentist every six months for routine cleanings and examination while you have braces. |
When to Use Veneers?
|
How Veneers Work
|
What is a Bridge?
|
Taking Care of Your Bridge
– Brush and floss with great care to clean where the crowns meet the tooth. – Flossing must be accomplished underneath the bridge on a daily basis. – Avoid eating or chewing on hard objects, food, or ice. – Make regular visits to your dentist to evaluate the condition of the crowns. |
When are Bridges Needed?
|
Types of Bridges
|
Aftercare
|
What is a Crown?
|
When are Crowns Needed?
The location of the tooth, the intensity of the bite, and your requirements as a patient are some of the factors used in deciding which type of crown is best for you. |
Placement Process
|
Aftercare
– Brush gently but thoroughly where the crown meets the gum – Avoid hard food or ice – Limit snacks – See your dentist regularly – If continual discomfort is experienced after placement, contact your dentist |
Types of Implants
– Made from titanium, covered with material that can attach to the jaw bone – Endosseous: placed within the jaw – Sub-periosteal: attached under the gum but over the jaw – Involves several visits – Either bridges or dentures are made to cover the implants |
Qualifications
– Sufficient jaw bone to support the implant – Lack of other medical complications |
Types of Gum Disease
Gingivitis is the earliest stage and affects only the gum tissue. At this stage, the disease is still reversible. If not treated, however, it may lead to a more sever condition. Periodontitis is the more advanced stage of periodontal diseases. The gums, bone and other structures that support the teeth become damaged. Teeth can become loose and fall out-or may have to be removed. At this stage, the disease may require more complex treatment to prevent tooth loss. Here is a step-by-step illustration of the process of gingivitis and periodontitis:
– People who smoke or chew tobacco are more likely to have gum diseases, and to have them more severely, than those who do not use any form of tobacco. – Poorly fitting bridges, malocclusion (badly aligned teeth) or defective restorations (fillings), can all contribute to plaque retentions and increase the risk of developing gum diseases. – Habits which place excessive biting forces on your teeth, such as clenching or grinding, may also accelerate the rate at which supporting bone is lost. – Poor diet may cause gum diseases to progress more rapidly or increase the severity of the condition, according to some researchers. There is also some evidence than an unbalanced diet makes mouth tissues less resistant to infection. – Pregnancy or use of oral contraceptives increases hormone levels which can cause gum tissues to react more sensitively to the toxins in plaque and accelerate growth or certain bacteria. The gums are more likely to become red, tender, and swollen and to bleed easily. – Systemic diseases, such as AIDS or diabetes, can lower the tissues’ resistance to infection, making gum diseases more sever. |
Symptoms
|
How Gum Disease is Treated
– Dentist will recommend procedures, for example: thorough cleaning, adjustment of bite, antibiotics, or minor surgery |
How to Prevent Gum Disease– Regular, professional cleaning of the mouth – Don’t wait until it hurts |
Why Remove Wisdom Teeth?Extraction of third molars can protect the overall health of the mouth. It is generally recommended when the following conditions occur:
|
When to Remove Wisdom Teeth?People between the ages of 16 and 19 should have their wisdom teeth evaluated. If they need to be removed, it should be considered before age 20 when generally fewer complications occur. At a younger age, tooth roots are not fully developed, the surrounding bone is softer, and there is less chance of damaging nearby nerves or other structures. There is also less surgical risk and healing is generally faster. Extractions of wisdom teeth may be performed by a general dentist. If your dentist anticipates any special care will be needed, he or she may refer you to an oral or maxillofacial surgeon. An oral or maxillofacial surgeon is a dentist who specializes in surgery and the removal of wisdom teeth. |
What to Expect?Before surgery, your dentist will explain what to expect, have you sign a consent form and give you personalized instructions to follow. Keep in mind these general items in order to help your surgery go smoothly. Wear loose, comfortable clothing and arrange to have someone be with you after surgery. Extraction can be performed under local conscious sedation or general anesthesia. Following surgery, you may experience some swelling and mild discomfort, which is part of the normal healing process. Cold compresses can help decrease the swelling and medication prescribed by your dentist can help decrease the pain. You may be instructed to drink only clear liquids following surgery and later progress to soft foods. Some patients experience numbness or tingling following surgery. Normal sensation usually returns in a short period of time. Occasionally, a dry socket occurs when the blood clot breaks down earlier than normal. A dressing placed in the socket protects it until the socket heals. Talk with your dentist about any questions that you have. It is especially important to let your dentist know, before surgery, of any illness that you have and medications that you are taking. If your general dentist has referred you to a specialist, they will both work together to provide you with the best and most efficient care. Keeping your teeth healthy – to a wise old age – is your dentist’s primary concern.
|
Aftercare
– Clear liquids, not hot, must be used in the diet for the first day – Soft foods can be consumed as tolerated – Brush all but the surgical site the first day, then all areas thereafter – Brush your tongue – Avoid rinsing and spitting the first day after surgery – Follow all special instructions given by your dentist |
 People usually think of a newborn baby as having no teeth. But the 20 primary teeth that will erupt in the next two and a half years are already present at birth in the baby’s jawbones. At birth, the crowns of the primary teeth are almost complete and the chewing surfaces of the permanent molars have begun to form. The front four teeth usually erupt first, beginning as early as six months after birth.
People usually think of a newborn baby as having no teeth. But the 20 primary teeth that will erupt in the next two and a half years are already present at birth in the baby’s jawbones. At birth, the crowns of the primary teeth are almost complete and the chewing surfaces of the permanent molars have begun to form. The front four teeth usually erupt first, beginning as early as six months after birth. Most children have a full set of 20 primary teeth by the time they are three years old. Primary teeth are just as important as permanent teeth, for chewing, speaking, and appearance. In addition, the primary teeth hold the space in the jaws for the permanent teeth.
Most children have a full set of 20 primary teeth by the time they are three years old. Primary teeth are just as important as permanent teeth, for chewing, speaking, and appearance. In addition, the primary teeth hold the space in the jaws for the permanent teeth. To prevent tooth decay and periodontal diseases, tooth brushing and flossing are needed daily to remove harmful plaque from your child’s teeth.
To prevent tooth decay and periodontal diseases, tooth brushing and flossing are needed daily to remove harmful plaque from your child’s teeth. Basic Dental Health Facts
Basic Dental Health Facts There are basically two types of mouth protectors:
There are basically two types of mouth protectors: If you have dental appliances such as orthodontic braces or bridgework, you should wear a mouth protector that has been fitted by a dentist.
If you have dental appliances such as orthodontic braces or bridgework, you should wear a mouth protector that has been fitted by a dentist.




 With the sealant deep within the pits and grooves of the enamel surface, normal eating habits can be maintained.
With the sealant deep within the pits and grooves of the enamel surface, normal eating habits can be maintained. Why do I need X-rays?
Why do I need X-rays? There are two types of bleaching procedures. Bleaching may be done completely in the dental office (known as “chairside bleaching”) or a system may be dispensed by the dentist to use at home (called “in-home bleaching”).
There are two types of bleaching procedures. Bleaching may be done completely in the dental office (known as “chairside bleaching”) or a system may be dispensed by the dentist to use at home (called “in-home bleaching”).
 Orthodontic treatment usually consists of applying braces to the teeth or using other appliances which gradually move the teeth or jaws into their correct position. Many of today’s braces are far less noticeable than those of the past.Braces consist primarily of brackets and interconnecting wires. Brackets (the part of the braces that hold the wires) are bonded to the teeth. Often, clear or tooth colored brackets are used for esthetics.
Orthodontic treatment usually consists of applying braces to the teeth or using other appliances which gradually move the teeth or jaws into their correct position. Many of today’s braces are far less noticeable than those of the past.Braces consist primarily of brackets and interconnecting wires. Brackets (the part of the braces that hold the wires) are bonded to the teeth. Often, clear or tooth colored brackets are used for esthetics.
 When braces are removed, it is usually necessary to wear a retainer for a period of time. A retainer keeps the teeth in their new, correct position until the tissues surrounding them stabilize.
When braces are removed, it is usually necessary to wear a retainer for a period of time. A retainer keeps the teeth in their new, correct position until the tissues surrounding them stabilize.










 Veneers are used to close gaps or cover teeth that are stained, poorly shaped, or slightly crooked. Even the most subtle change in your smile can make a dramatic difference in the way you look and feel. When you feel and look good, you project a confident self-image. So, make the most of your smile. Ask your dentist what veneers can do for you.
Veneers are used to close gaps or cover teeth that are stained, poorly shaped, or slightly crooked. Even the most subtle change in your smile can make a dramatic difference in the way you look and feel. When you feel and look good, you project a confident self-image. So, make the most of your smile. Ask your dentist what veneers can do for you.
 A bridge is a replacement tooth that is supported and attached by a crown on either side of the space. The two side teeth or (anchor teeth) are prepared to provide support the bridge).
A bridge is a replacement tooth that is supported and attached by a crown on either side of the space. The two side teeth or (anchor teeth) are prepared to provide support the bridge).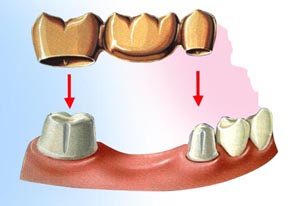 A bridge is made of very strong materials, but nothing as strong as natural tooth structure. If normal care and precautions and care are taken, a bridge can last for many years.
A bridge is made of very strong materials, but nothing as strong as natural tooth structure. If normal care and precautions and care are taken, a bridge can last for many years.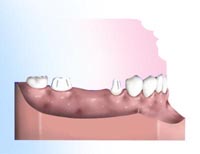 To replace a missing tooth with a conventional three-unit bridge, teeth adjacent to the gap are prepared.
To replace a missing tooth with a conventional three-unit bridge, teeth adjacent to the gap are prepared.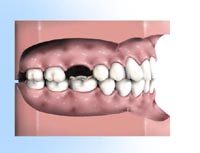 Appearance immediately after a tooth is lost.
Appearance immediately after a tooth is lost. When a tooth is not replaced, the remaining teeth can drift out of position. This can lead to cavities and gum disease.
When a tooth is not replaced, the remaining teeth can drift out of position. This can lead to cavities and gum disease. Bridges come in two main types. Fixed bridges or Removable bridges.
Bridges come in two main types. Fixed bridges or Removable bridges.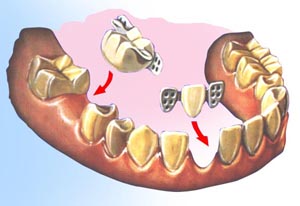 Some fixed bridges cement over a tooth, others cement to the outside surface of a tooth.
Some fixed bridges cement over a tooth, others cement to the outside surface of a tooth. Crowns are made of metal, ceramic, or a combination of the two and require very high temperatures in converting the carved was representation into the finished product. Crowns are fitted to a model of your mouth that is made at the time the teeth are prepared in your mouth. The crown is shaped and fitted to this model in the laboratory before the dentist tries it in your mouth. This process ensures that the crown will have a fit and appearance that will last for many years.
Crowns are made of metal, ceramic, or a combination of the two and require very high temperatures in converting the carved was representation into the finished product. Crowns are fitted to a model of your mouth that is made at the time the teeth are prepared in your mouth. The crown is shaped and fitted to this model in the laboratory before the dentist tries it in your mouth. This process ensures that the crown will have a fit and appearance that will last for many years. When a tooth is fractured, severely damaged by decay, or has a large old filing, a crown (also called a cap) is often placed. A crown strengthens the tooth, protects the remaining tooth structure and can improve appearance.
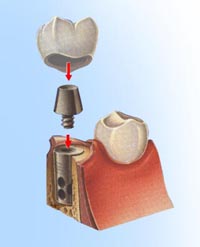
When a tooth is fractured, severely damaged by decay, or has a large old filing, a crown (also called a cap) is often placed. A crown strengthens the tooth, protects the remaining tooth structure and can improve appearance.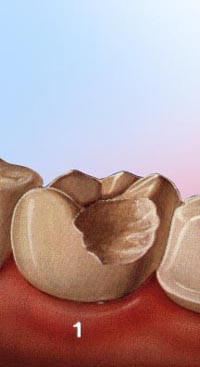 Step 1The tooth is prepared to accept a crown. All odd fillings, decay, and unsupported tooth is removed to ensure a solid foundation for the new crown. An impression of the prepared tooth is made, and the appropriate shade of the crown is determined to match the patient’s tooth color.
Step 1The tooth is prepared to accept a crown. All odd fillings, decay, and unsupported tooth is removed to ensure a solid foundation for the new crown. An impression of the prepared tooth is made, and the appropriate shade of the crown is determined to match the patient’s tooth color.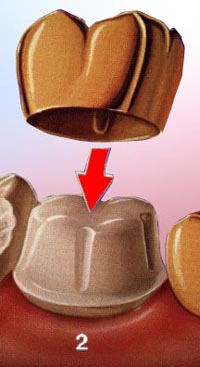 Step 2A temporary crown is made, usually of tooth-colored plastic, to cover and protect the tooth until the crown is ready.
Step 2A temporary crown is made, usually of tooth-colored plastic, to cover and protect the tooth until the crown is ready.
 Step 3The crown is tried on for a fit, shape, and color. The bite is checked and adjusted. If all is satisfactory, the crown is bonded to the tooth.
Step 3The crown is tried on for a fit, shape, and color. The bite is checked and adjusted. If all is satisfactory, the crown is bonded to the tooth.
 – Artificial substitutes for natural tooth roots
– Artificial substitutes for natural tooth roots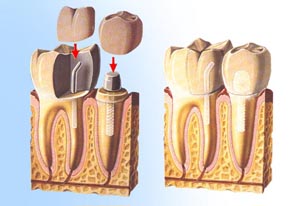 – Someone in good health
– Someone in good health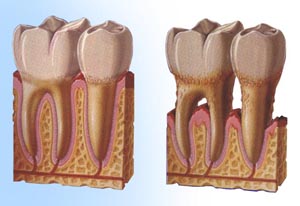 While there are many forms of gingival and periodontal diseases, the most common type are gingivitis and adult periodontitis.
While there are many forms of gingival and periodontal diseases, the most common type are gingivitis and adult periodontitis. 1. Healthy gingival (gum tissue) and bone anchor the teeth firmly in place.
1. Healthy gingival (gum tissue) and bone anchor the teeth firmly in place. 2. Gingivitis develops as toxins in plaque irritate the gums, making them red, tender, swollen and likely to bleed easily.
2. Gingivitis develops as toxins in plaque irritate the gums, making them red, tender, swollen and likely to bleed easily.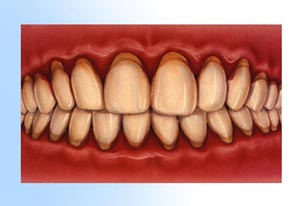 3. Periodontitis occurs when toxins destroy the tissues that anchor the teeth in the bone. Gums become detached from the teeth, forming pockets that fill with more plaque. Tooth roots are exposed to plaque and become susceptible to decay and sensitive to cold and touch.
3. Periodontitis occurs when toxins destroy the tissues that anchor the teeth in the bone. Gums become detached from the teeth, forming pockets that fill with more plaque. Tooth roots are exposed to plaque and become susceptible to decay and sensitive to cold and touch.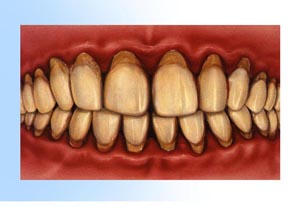 4. Advanced periodontitis is present when the teeth lose more attachment because the supporting bone is destroyed. Unless treated, the affected teeth frequently become loose and may fall out or require removal by a dentist.
4. Advanced periodontitis is present when the teeth lose more attachment because the supporting bone is destroyed. Unless treated, the affected teeth frequently become loose and may fall out or require removal by a dentist.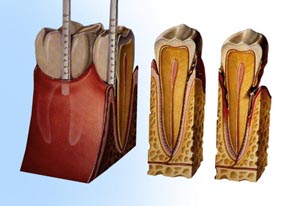 Although gum diseases are caused by plaque, a number of other factors can increase the risk, severity, and speed of development of the condition.
Although gum diseases are caused by plaque, a number of other factors can increase the risk, severity, and speed of development of the condition.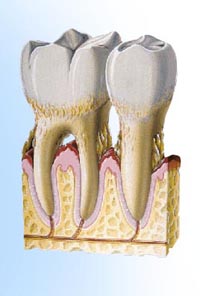 – Depends on the stage you are in
– Depends on the stage you are in Wisdom teeth only partially erupt. This leaves an opening for bacteria to enter around the tooth and cause an infection. Pain, swelling, jaw stiffness, and general illness can result.
Wisdom teeth only partially erupt. This leaves an opening for bacteria to enter around the tooth and cause an infection. Pain, swelling, jaw stiffness, and general illness can result. Impacted wisdom teeth may continue growing without enough room, damaging adjacent teeth.A fluid-filled sac (cyst) or tumor forms, destroying surrounding structures such as bone or tooth roots.
Impacted wisdom teeth may continue growing without enough room, damaging adjacent teeth.A fluid-filled sac (cyst) or tumor forms, destroying surrounding structures such as bone or tooth roots.